“Unveiling not a very rare case of male infertility.“
Retrograde ejaculation is a medical condition which is characterised by propulsion of seminal fluid from posterior urethra into urinary bladder. Clinically, it is diagnosed by absence of sperm with low/no ejaculate volume during semen analysis test. This is called “dry ejaculation”. There is no problem in erection or orgasm. Typically, such men complaint of cloudy coloured urine after sexual activity.
Pathophysiology
Ejaculation is a complex process controlled by a spinal reflex, and is triggered by tactile stimulation caused by sympathetic mechanoreceptors within the penis.
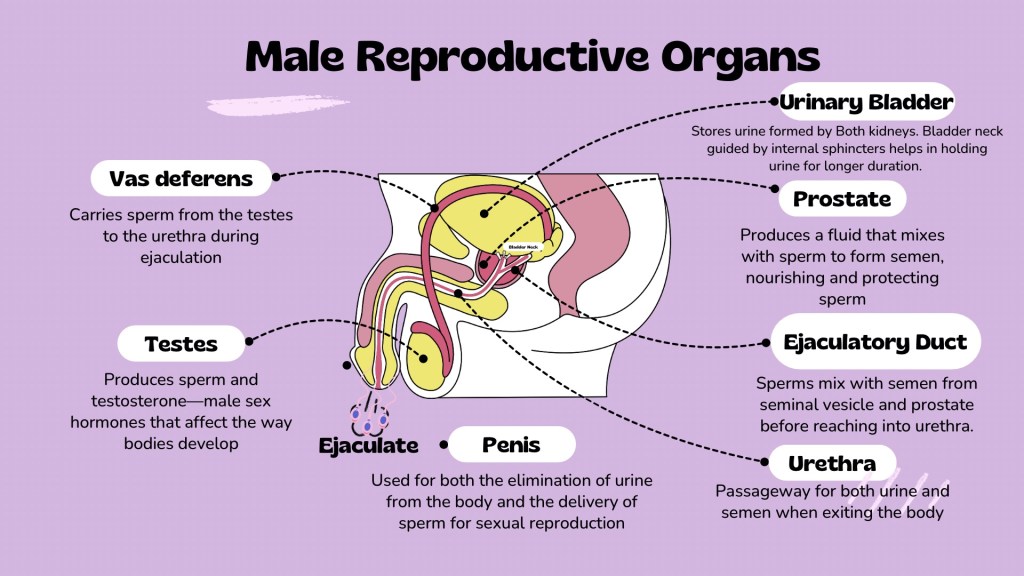
Ejaculation occurs in two phases: 1) emission, and 2) expulsion resulting through contraction of the penile musculature.
During the expulsive phase of semen, the bladder neck ( also known as internal urethral sphincter) is being closed to prevent the reflux of semen into the bladder. This closure of the bladder neck is under sympathetic control. Failure of closure of the bladder neck results in reflux of semen into the bladder which is known as retrograde ejaculation.
Causes
- Surgeries like retroperitoneal pelvic lymph node dissection, TURP, etc.
- Medical conditions like diabetics, multiple sclerosis, etc.
- Trauma to spinal cord
Diagnosis
Retrograde ejaculation accounts for less than 2% of cases of subfertility presenting to a fertility clinic.
Semen analysis reveals low ejaculate volume with no sperm count. Post ejaculate urine (PEU) on microscopic analysis show presence of dead or alive sperms.
Treatment
Medical Treatment: Sympathomimetic drugs (Ephedrine sulphate, Pseudoephedrine hydrochloride, Synephrine, Phenylpropanolamine, Midrodrin, phenylephedrine hydrochloride, isopropamide iodide, etc.), Anticholinergics drug (Imipramine hydrochloride, Chlorpheniramine maleate, Brompheniramine maleate), Acupuncture and traditional Chinese medicines.
Surgical Treatment: aims at restoring integrity of the bladder neck, when medical treatment fails.
Assisted reproductive treatment (ART) i.e. IUI or IVF-ICSI: The patients who dont get benefited from medical or surgical treatment, can undergo ART. It aims at extracting sufficient viable sperms from post-ejaculatory urine (after alkalising the urine) for insemination (IUI), IVF, or intracytoplasmic sperm injection (ICSI). If sufficient good quality sperms are not retrieved from urine sample, Testicular sperm aspiration (TESA) can be done.
Real example of Treatment of retrograde ejaculation through ART services
Lets have a look on a real case experience of an infertile couple with retrograde ejaculation coming to my fertility OPD:
A couple, Mrs. X, 28 years old; and Mr. Y, 32 years old with married life of 3 years came to my OPD with primary infertility. Mrs. X was short statured with 145 cm height, BMI 26.16 kg/m2, normal menstrual cycle, and AMH 2.4 ng/ml. Her uterine size was also small, as per her built. Mr. Y was average in built, and was a known case of irritable bowel disease and pulmonary Tuberculosis in childhood, for which he took antitubercular treatment for 6 months. Mr. X was already diagnosed with retrograde ejaculation by his previous andrologist and was prescribed certain medication which failed to benefit him much.
We ordered a repeat Semen analysis and post ejaculatory urine (PEU) analysis after prescribing him alkaliser from one day prior. To be precise, tab Sodium bicarbonate 500mg 2 tab were given at 6pm, 12 MN, 6 am, and, patient was called at 10 am for semen analysis and PEU. Semen analysis suggested azoospermia and PEU showed only 1-2 motile sperms.
Detailed couple counselling was done for the need of TESA- ICSI.
Mrs X underwent IVF-ISCI stimulation for 10 days with HMG dose of 300IU/ day (PPOS protocol) with total Antral follicle count (AFC) of 10 on day-2 of periods. Eight oocytes were retrived , out of which 6 were mature oocytes (MIIs). TESA (testicular sperm aspiration) was done, and aspirated sperms were used for ICSI. Five oocytes were fertilized, 5 cleaved to day 3 embryos. Two day 3 embryos (10cA, 8cA) were freezed and rest three were taken to day-5. One day 5 embryo was freezed (1 x 3BB), one was arrested, one was slow growing, so taken to day 6 and freezed (1 x 3 BB).
Frozen embryo transfer was done. The two day 3 embryos were taken for extended culture to day 5. Only one embryo grew, the other arrested. So, another straw of day 5 embryo was thawed and two day 5 embryos were transferred.
Fifteen days later, her beta hCG was 2629.0 miu/ml. The six weeks early pregnancy ultrasound showed singleton intrauterine live pregnancy. Eighteen weeks ultrasound suggest ongoing live healthy pregnancy.
Summary
Retrograde ejaculation is a condition affecting male fertility and not many clinician are aware about it. Expert guidance is required so as to approach such cases in professional and ethical manner.
Post ejaculatory urine analysis usually help in making the diagnosis. ART services are required in most of the case in which fertility is desired.
Leave a comment